
This treatment works by delivering radiofrequency waves to deeply penetrate and heat the eyelids to loosen blockages causing your dry eye symptoms. This treatment promotes a healthy tear film, helping you achieve comfortable vision without symptoms of dry eye.
As an added benefit, it can also promote collagen production in your skin to reduce fine lines and wrinkles giving you a more youthful appearance.
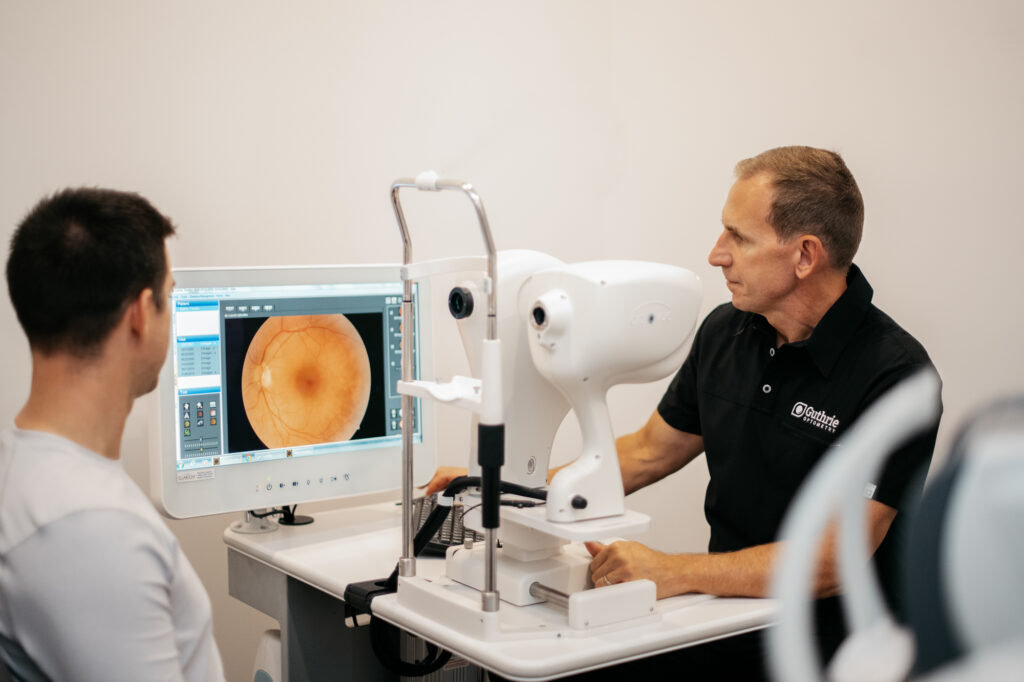
We are committed to providing you with the most thorough eye examination available today. Guthrie Optometry is able to offer the most advanced retinal health and optic nerve screening, the i-Wellness OCT. This technology is one of the most important eye care tools used to detect eye disease and prevent vision loss. Early detection of ocular conditions like macular degeneration and diabetic retinopathy allow for prompt treatment and ultimately better vision long term.
Guthrie Optometry believes i-Wellness is an opportunity for patients to be proactive with their eye health and recommends periodic retinal OCT screenings. The i-Wellness scan in conjunction with retinal photography and a microscopic evaluation by Dr. Guthrie provides the ultimate in retinal health examinations.

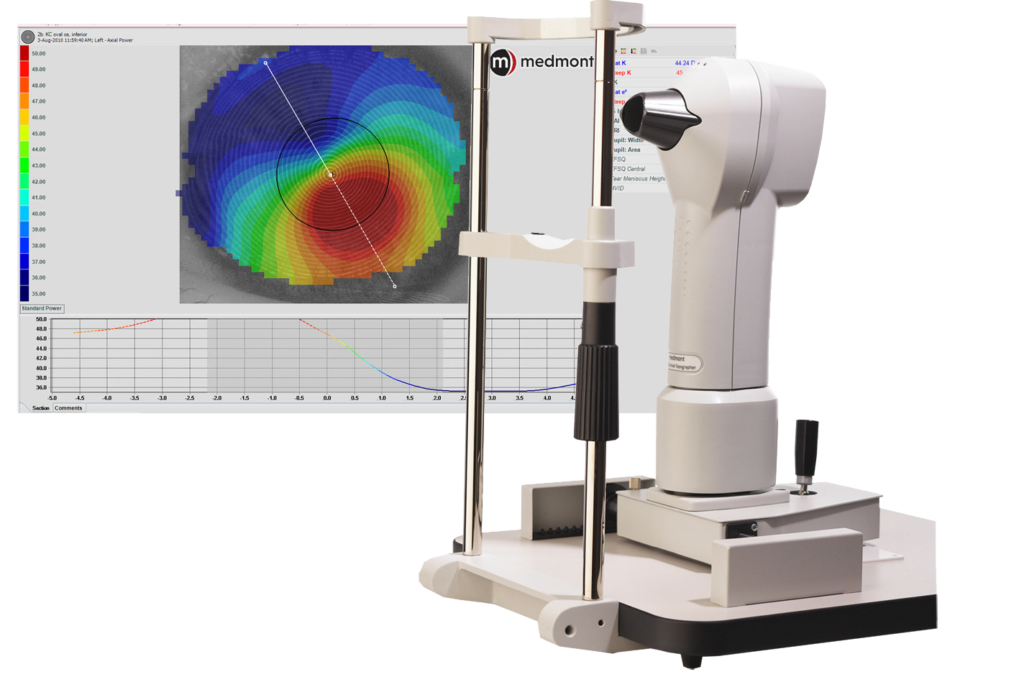
Topographer Meidmont E 300 is diagnostic instrument used to measure the exact curvature of the cornea which allows for advanced contact lens fittings and aids in the diagnosis of corneal disease like keratoconus.

The Octopus 900 Visual Field Analyzer represents the most complete projection perimeter available today. Testing the patients peripheral visual field is a key element in the diagnosis and management of many ocular conditions.
It features the fastest test strategy and a full threshold test within 2.5 minutes. Speed combined with reliability make the Octopus 900 visual field an important tool for Dr. Guthrie to manage ocular disease.
©2025 Guthrie Optometry | All rights reserved.
 A Christopher Pressey Website
A Christopher Pressey Website